The purpose of this article is not to make a recommendation on the use (or not use) of the drug Brexpiprazole (brand name: Rexulti) that has recently been approved by Health Canada for the treatment of dementia-related agitation and aggression among individuals with Alzheimer’s disease. Instead, this article hopes to present facts currently available about this drug to help those diagnosed with Alzheimer’s disease and their families make an informed decision regarding its potential usage.
It’s crucial to emphasize that this medication isn’t designed to cure or slow down the advancement of Alzheimer’s disease. It is NOT a cure for Alzheimer’s disease and other related dementias. Instead, its purpose is to “manage difficult behaviors” often exhibited by individuals with Alzheimer’s disease.
Brexpiprazole (Rexulti)
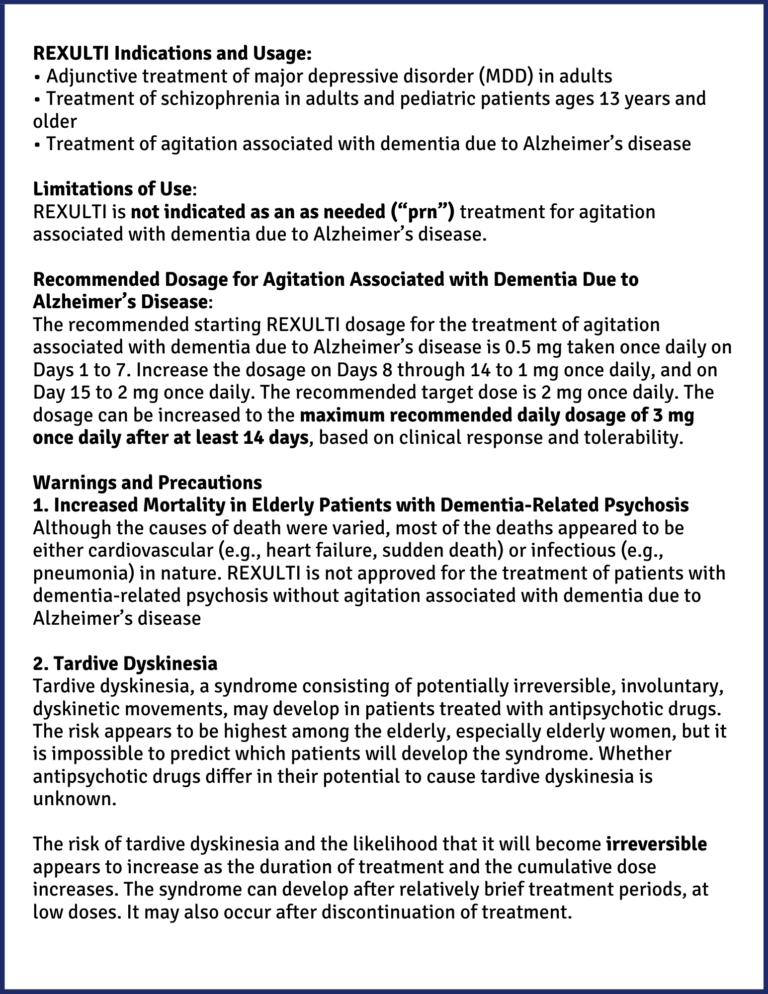
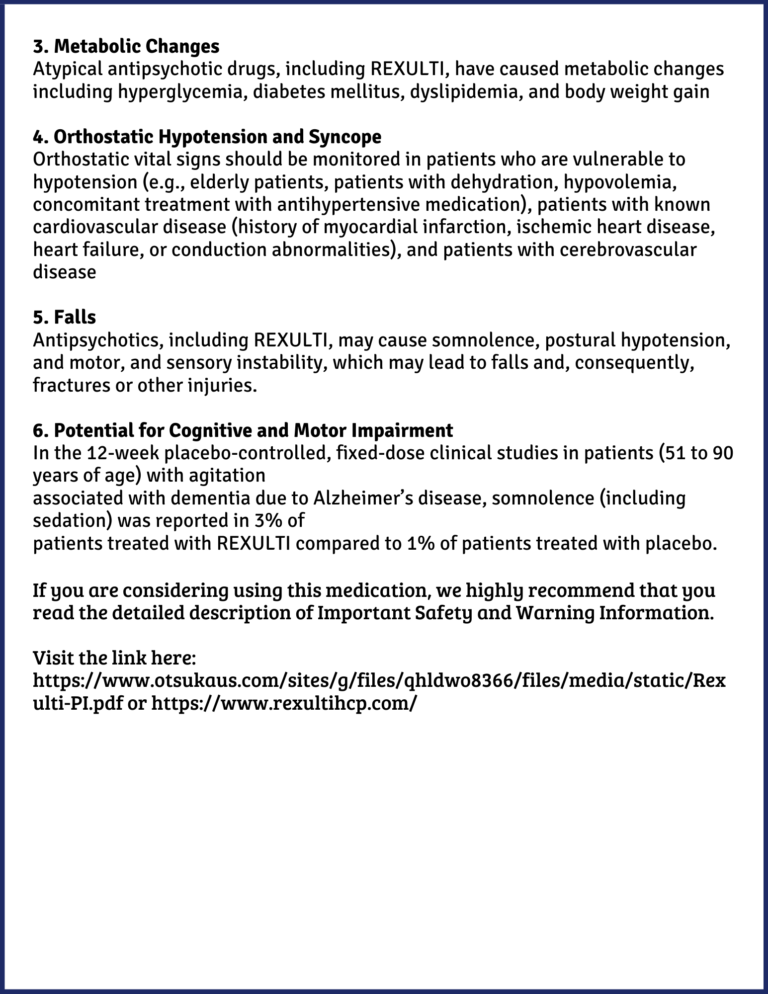
Rexulti (oral tablets) is classified as an antipsychotic medication. It has been available in the market in Canada since February 2017 for the treatment of schizophrenia and major depressive disorder. It is manufactured by Otsuka Pharmaceutical Canada Inc. and Lundbeck Canada Inc. The information that follows was taken and quoted directly from the manufacturer’s website. Below is information we deem relevant for potential prescribers and users need to be aware of. These are just some of the highlights.
Patient Well-being and Person-Centred Care
ALL drugs have their intended use, side effects and risks.
Drugs and their metabolites interact with other drugs that, at best, can “neutralize” each other’s effect in the system, rendering both drugs “ineffective”. In more severe cases, such interactions can pose risks and harm to individuals.
In instances of “polypharmacy,” a term denoting the concurrent use of multiple medications often observed in older individuals, it becomes increasingly crucial to maintain hypervigilance in understanding the mechanisms of each drug, their potential side effects, and their interplay, particularly in individuals with dementia.
Most importantly, a fundamental aspect to remember is the purpose behind medication usage. Medications alleviate a person’s suffering by treating or curing an infection or illness and managing symptoms that negatively impact their quality of life.
At Dementia Solutions we strive to advocate and educate caregivers, healthcare professionals and the wider community that there is a meaning behind the behaviour. Among people living with dementia, their behaviour (e.g., agitation, shouting, wondering, repetitive questions, anger, or withdrawal from others) is their means of communication. Behaviour is their form of communication.
Often, they could be experiencing delirium because of an untreated infection. In other cases, they could be in pain, feeling cold, and didn’t get enough sleep, lonely, bored missing their loved ones or a combination of the above.
The question then is: If we silence their behaviour through medication, we may be in effect, taking away their last means to communicate and prevent them from letting us know there is something wrong that needs urgent attention.
Medications are quick and easy solutions to manage difficult behaviours; but are we managing their symptoms for their well-being and comfort?
Hugs not drugs
“Hugs not drugs” started in the 1980s as part of a campaign against drugs. However, this catchy slogan is now being adapted in many care settings for older adults as a way to support difficult behaviours for people with dementia.
According to a 2013 Vancouver Sun article written by Heather, Campbell, BC Care Providers Association Director of Policy and Research, on exploring non-pharmacological alternatives to dementia-related behaviours, “While these medications can be a quick fix for health care professionals managing the aggressive and restless behaviours of dementia, they are not the preferred solution. Antipsychotics not only strip seniors of their quality of life, but they also put the elderly at an increased risk of falls, hip fractures, stroke, heart attack and death.”
At Dementia Solutions, we are not “anti-pharmaceuticals.” However, it’s important to understand that drugs are not the “be-all and end-all” in healthcare. The term “healthcare’” itself inherently conveys its primary focus: prioritizing the promotion of health and providing compassionate care. Pharmacology is a tool in our toolbox in healthcare but it is not the only tool. Human beings possess a complexity far beyond the scope of pharmacological interventions alone.
Finally, regarding the utilization of medications for addressing behaviors associated with dementia, it is essential to undertake due diligence. Conduct extensive research and diligently pose inquiries to healthcare experts such as physicians, pharmacists, and nurse practitioners. Continue seeking clarification until you have a comprehensive understanding of the answers provided. Accountability should be a shared responsibility for all.
At Dementia Solutions, we’ve made it our mission to demystify dementia behaviour and continue to explore person-centred, creative, non-pharmacological solutions to manage dementia-related behaviours. We believe that awareness creation and skill-building through education is the most effective and powerful tool we have to promote and maintain the well-being of both the person with dementia and their caregiver. You may find this Meaning Behind the Behaviour Story helpful.
If you need support in your caregiving experience or would like to learn more about our educational opportunities, please reach out to us at Info@DementiaSolutions.ca and we would be more than happy to support you.
DISCLAIMER:
The contents of this blog are provided for information purposes only. They are not intended to replace clinical diagnosis or medical advice from a health professional.